The ketogenic diet has gained attention as a potential approach for managing diabetes. This low-carbohydrate, high-fat eating plan aims to shift the body into a state of ketosis, where it burns fat for fuel instead of glucose. For individuals with type 2 diabetes, the keto diet may offer benefits in blood sugar control and weight management.
Research has shown that following a ketogenic diet can help lower blood sugar levels and reduce insulin needs in people with type 2 diabetes. By drastically reducing carbohydrate intake, the diet minimizes spikes in blood glucose that typically occur after meals. This can lead to improved glycemic control and potentially decrease the need for diabetes medications.
While the keto diet shows promise for diabetes management, it’s important to approach it with caution. The diet’s strict carbohydrate limitations may pose challenges for some individuals, and close monitoring by a healthcare provider is essential. As with any significant dietary change, people with diabetes should consult their doctor before starting a ketogenic eating plan to ensure it’s appropriate for their specific health needs.
Understanding Keto Diet and Diabetes
The ketogenic diet and diabetes have a complex relationship. This high-fat, low-carb eating plan can impact blood sugar levels and insulin sensitivity in different ways for various types of diabetes.
The Fundamentals of Keto Diet
The ketogenic diet drastically reduces carbohydrate intake, typically to less than 50 grams per day. It emphasizes high fat consumption, moderate protein, and minimal carbs. This macronutrient balance forces the body into a state of ketosis.
In ketosis, the body burns fat for fuel instead of glucose. This metabolic shift can lead to weight loss and improved insulin sensitivity in some individuals.
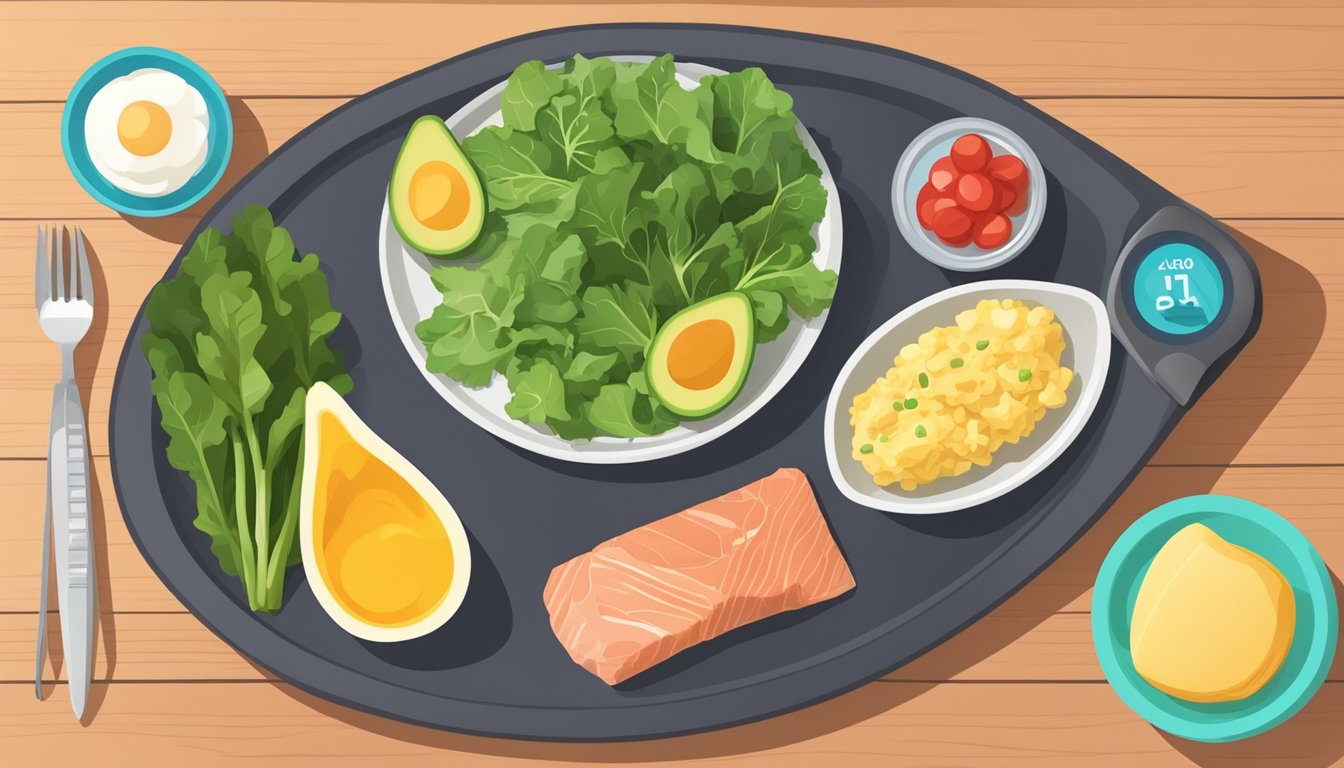
Key foods on the keto diet include:
- Meats and fatty fish
- Eggs
- High-fat dairy
- Nuts and seeds
- Avocados and low-carb vegetables
Diabetes Overview
Diabetes is a chronic condition characterized by high blood sugar levels. It occurs when the body either can’t produce insulin (Type 1) or can’t effectively use the insulin it produces (Type 2).
Insulin is crucial for regulating blood glucose. In diabetes, this regulation is impaired, leading to potential complications if left unmanaged.
Common symptoms of diabetes include:
- Increased thirst and frequent urination
- Fatigue
- Blurred vision
- Slow-healing wounds
Different Types of Diabetes and Their Responses to Keto
Type 1 Diabetes: This autoimmune condition requires lifelong insulin therapy. The keto diet may help stabilize blood sugar levels, but it requires careful monitoring to prevent diabetic ketoacidosis.
Type 2 Diabetes: This form often responds well to the keto diet. The low-carb approach can lead to better blood sugar control and reduced medication needs in some cases.
Research shows the keto diet can improve insulin sensitivity in Type 2 diabetes. However, it’s crucial for individuals with diabetes to consult healthcare providers before starting any new diet regimen.
Gestational Diabetes: Pregnant women with this condition should approach the keto diet with caution due to potential risks to fetal development.
Keto Diet and Type 1 Diabetes Management
The ketogenic diet can potentially benefit type 1 diabetes management, but it requires careful consideration and medical supervision. This approach aims to improve blood glucose control and reduce insulin needs.
Managing Blood Glucose Levels
A ketogenic diet may help stabilize blood glucose levels in type 1 diabetes. By limiting carbohydrate intake, this diet can reduce the need for insulin injections and potentially lower the risk of hypoglycemic episodes.
Some studies have shown improved A1c levels in type 1 diabetics following a ketogenic diet. The diet’s emphasis on fat and protein can lead to more consistent blood sugar readings throughout the day.
Insulin sensitivity may also improve on a ketogenic diet. This can result in more effective glucose control with smaller insulin doses.
Potential Risks of Keto for Type 1 Diabetes
While the ketogenic diet offers potential benefits, it also carries risks for type 1 diabetics. The most significant concern is the increased risk of diabetic ketoacidosis (DKA).
DKA occurs when blood ketone levels become dangerously high. Type 1 diabetics are already prone to this condition, and a ketogenic diet may exacerbate this risk.
Careful monitoring of blood glucose and ketone levels is crucial. Regular check-ups with a healthcare provider are essential to ensure safety and adjust insulin dosages as needed.
Personalized Keto Dietary Approaches
Implementing a ketogenic diet for type 1 diabetes requires a personalized approach. Each individual’s insulin needs, lifestyle, and health status must be considered.
A gradual transition to a ketogenic diet is often recommended. This allows for careful monitoring of blood glucose levels and insulin adjustments.
Collaboration with a healthcare team, including an endocrinologist and registered dietitian, is crucial. They can help create a tailored meal plan and adjust insulin regimens to suit the individual’s needs.
Regular blood work and monitoring of A1c levels can help track progress and ensure the diet remains safe and effective over time.
Keto Diet’s Role in Type 2 Diabetes
The ketogenic diet has shown promising results in managing type 2 diabetes. It impacts weight loss, insulin sensitivity, and blood sugar control, offering potential benefits for diabetic patients.
Weight Loss and Insulin Resistance
The keto diet promotes rapid weight loss, which can significantly improve insulin resistance in type 2 diabetics. By restricting carbohydrates, the body enters ketosis, burning fat for fuel instead of glucose.
This metabolic shift often leads to a reduction in body fat, particularly visceral fat. Decreased visceral fat is associated with improved insulin sensitivity and better glucose regulation.
Studies have shown that keto dieters with type 2 diabetes experience substantial weight loss within the first few months. This weight reduction can lead to a decrease in medication requirements for some patients.
Keto Diet as a Tool for Diabetes Management
The ketogenic diet’s low-carb approach helps stabilize blood sugar levels in type 2 diabetics. By limiting carbohydrate intake, the diet reduces glucose spikes after meals.
Research indicates that a ketogenic diet can lead to significant reductions in HbA1c levels. Some studies have reported decreases of 1% or more in HbA1c within 3-6 months of starting the diet.
The diet may also improve other markers of metabolic health, such as triglycerides and HDL cholesterol. These changes can contribute to better overall diabetes management and reduced cardiovascular risk.
Monitoring and Adherence
While the keto diet shows promise, close monitoring is crucial for diabetic patients. Regular blood glucose checks and medication adjustments may be necessary, especially in the early stages of the diet.
Adherence can be challenging due to the diet’s restrictive nature. Patients may struggle with eliminating high-carb foods and maintaining ketosis long-term.
Healthcare providers should work closely with patients to ensure proper nutrition and prevent potential side effects. Regular check-ups and blood tests can help track progress and make necessary adjustments to the diet or medication regimen.
Nutritional Aspects of the Ketogenic Diet
The ketogenic diet relies on a specific macronutrient balance to induce nutritional ketosis. This approach emphasizes high fat intake, moderate protein consumption, and strict carbohydrate restriction.
Macronutrient Distribution & Choices
A typical ketogenic diet consists of 70-80% calories from fat, 15-20% from protein, and only 5-10% from carbohydrates. This translates to approximately 20-50 grams of carbs per day. Fat sources include avocados, nuts, seeds, olive oil, and fatty fish. Protein comes from eggs, meat, and dairy.
Carbohydrate intake focuses on low-glycemic vegetables like leafy greens, broccoli, and cauliflower. Fruits are limited due to their sugar content. The diet excludes grains, legumes, and starchy vegetables.
Importance of Fiber and Quality Fat Intake
Despite carbohydrate restriction, fiber remains crucial for gut health and satiety. Fibrous vegetables, chia seeds, and flaxseeds can help meet daily fiber needs.
Quality fat intake is essential. The diet emphasizes healthy fats like monounsaturated and polyunsaturated fats. These include omega-3 fatty acids found in fish oil and flaxseed. Saturated fats from coconut oil and grass-fed butter are also included.
Processed and trans fats are discouraged due to their negative health impacts.
Adapting to Energy Expenditure
The ketogenic diet’s calorie intake should align with individual energy needs. Active individuals may require more calories to support their activity levels.
Protein intake may need adjustment based on exercise intensity and muscle-building goals. Athletes might increase protein slightly while maintaining ketosis.
Monitoring ketone levels through blood or urine tests helps ensure the diet is effectively inducing ketosis. Adjustments to macronutrient ratios may be necessary to achieve and maintain this metabolic state.
Electrolyte balance is crucial, as the diet can lead to increased fluid loss. Adequate sodium, potassium, and magnesium intake helps prevent electrolyte imbalances and associated symptoms.
Health Implications Beyond Glycemic Control

The ketogenic diet’s effects extend beyond blood sugar management. It influences various aspects of health, including cardiovascular markers, weight, and other conditions.
Cholesterol Levels and Cardiovascular Health
The high-fat nature of the ketogenic diet raises questions about its impact on cholesterol and heart health. Research shows mixed results. Some studies report increases in LDL cholesterol, often considered “bad” cholesterol. Others note improvements in HDL cholesterol and triglyceride levels.
A 2020 meta-analysis found that keto diets led to greater reductions in total cholesterol and increases in HDL compared to low-fat diets. Triglycerides also decreased significantly.
It’s important to note individual responses vary. Some people may experience unfavorable changes in lipid profiles. Regular monitoring is recommended for those following a ketogenic diet long-term.
Keto Diet’s Impact on Obesity and Non-Diabetic Conditions
The ketogenic diet shows promise for weight loss in obese individuals. A 2013 study found that a very low-carbohydrate ketogenic diet was more effective for weight loss than a low-glycemic index diet.
Beyond obesity, keto diets have been explored for other health conditions:
- Epilepsy: Used as a treatment for drug-resistant epilepsy in children
- Neurological disorders: Potential benefits for Alzheimer’s and Parkinson’s disease
- Cancer: Some research suggests it may complement certain cancer therapies
While promising, more research is needed to fully understand the diet’s effects on these conditions.
The Debate on Long-Term Effects
The long-term health implications of following a ketogenic diet remain a topic of debate. Proponents argue that it can lead to sustained weight loss and improved metabolic health. Critics raise concerns about potential nutrient deficiencies and effects on gut health.
A 5-year study by Virta Health showed sustained benefits for type 2 diabetes management. However, long-term adherence can be challenging for some individuals.
Potential side effects include:
- Kidney stones
- Bone loss
- Gastrointestinal issues
More long-term studies are needed to fully assess the diet’s safety and efficacy over extended periods.
Dietary Patterns and Keto Integration
Integrating a ketogenic diet into existing dietary patterns requires careful consideration of nutritional balance, individual needs, and sustainability. Proper implementation can complement diabetes management strategies for some individuals.
Transitioning to and Sustaining a Ketogenic Lifestyle
Transitioning to a ketogenic diet involves gradually reducing carbohydrate intake while increasing healthy fats. Start by cutting out refined sugars and grains. Replace them with low-carb vegetables, nuts, seeds, and high-quality proteins.
Monitor blood glucose levels closely during this transition. Adjust medication as needed under medical supervision.
To sustain a ketogenic lifestyle, focus on meal planning and preparation. Stock your kitchen with keto-friendly foods. Learn to read nutrition labels carefully.
Incorporate a variety of fats, including avocados, olive oil, and fatty fish. This helps prevent nutrient deficiencies and maintains diet adherence.
Stay hydrated and supplement electrolytes as needed. This can help mitigate potential side effects like the “keto flu.”
Comparing Keto with Other Diets
The ketogenic diet differs significantly from other popular dietary patterns. Unlike the Mediterranean diet, which emphasizes whole grains and fruits, keto severely restricts carbohydrates.
The Atkins diet shares similarities with keto in its low-carb approach. However, Atkins allows for a gradual increase in carb intake over time.
Low-carb diets generally permit more carbohydrates than keto. They may be easier to sustain long-term for some individuals.
Plant-based diets can be adapted to fit ketogenic principles. This requires careful planning to ensure adequate protein and fat intake while limiting carbs.
Each dietary pattern offers unique benefits and challenges for diabetes management. The optimal choice depends on individual health goals, preferences, and metabolic responses.
Customization for Dietary Restrictions
Ketogenic diets can be adapted to accommodate various dietary restrictions. For vegetarians, emphasize plant-based fats like coconut oil, nuts, and seeds. Include eggs and dairy if allowed.
Vegans can rely on avocados, olives, and plant oils for fats. Incorporate low-carb plant proteins such as tofu and tempeh.
Those with food allergies or intolerances may need to explore alternative fat sources. For example, individuals with dairy allergies can use coconut-based products as substitutes.
Gluten-free ketogenic diets naturally exclude wheat-based products. Focus on whole foods like meats, fish, eggs, and low-carb vegetables.
Customize meal plans to meet specific nutritional needs. Work with a registered dietitian to ensure proper nutrient intake while maintaining ketosis.
Special Considerations and Contraindications

While the ketogenic diet shows promise for managing diabetes, certain individuals may face risks or require special attention. Careful monitoring and personalized adjustments are crucial for safe implementation.
Identifying Individuals at Risk
Patients with a history of pancreatitis or gallbladder disease should exercise caution when considering a ketogenic diet. The high fat content may exacerbate these conditions. Those with kidney problems may need to limit protein intake, which can be challenging on a keto diet.
Individuals with a history of eating disorders should approach the diet with caution, as its restrictive nature could trigger unhealthy behaviors. People with thyroid disorders may experience changes in medication needs due to the diet’s effect on hormone levels.
Pregnant women and those with type 1 diabetes should consult their healthcare providers before starting a ketogenic diet. The American Diabetes Association emphasizes the importance of individualized nutrition plans for diabetes management.
Navigating Through Hypoglycemia and Ketoacidosis
Diabetic patients on a ketogenic diet must be vigilant about blood sugar levels. Hypoglycemia can occur if medication dosages are not adjusted appropriately. Regular blood glucose monitoring is essential, especially during the initial adaptation phase.
Diabetic ketoacidosis (DKA) is a serious concern for type 1 diabetics. While nutritional ketosis differs from DKA, the risk increases if insulin is inadequate. Symptoms like excessive thirst, frequent urination, and fruity-smelling breath warrant immediate medical attention.
To minimize risks:
- Monitor blood glucose and ketone levels regularly
- Adjust medications under medical supervision
- Stay hydrated and maintain electrolyte balance
- Recognize early signs of complications
Adjustments for Special Populations
Elderly individuals may require modifications to prevent muscle loss and maintain bone health. Increasing protein intake and incorporating resistance exercises can help preserve muscle mass.
Children and adolescents with diabetes need careful consideration before starting a ketogenic diet. Growth and development requirements must be met, and close monitoring by a pediatric endocrinologist is crucial.
Athletes with diabetes may need to adjust their approach to ensure adequate energy for performance. Carbohydrate intake may need to be strategically timed around training sessions.
Patients with comorbidities like fatty liver disease or cardiovascular issues should work closely with their healthcare team. The diet’s impact on cardiometabolic risk factors varies among individuals and requires personalized management.
Support and Resources
Managing diabetes while following a ketogenic diet requires knowledge, tools, and a support system. Proper education and guidance are essential for successful implementation and long-term adherence.
Education and Diabetes Management Tools
Diabetes management on a ketogenic diet involves understanding carbohydrate counting, blood sugar monitoring, and ketone testing. The American Diabetes Association offers resources on nutrition therapy and blood sugar management. Many diabetes education programs now include information on low-carbohydrate approaches.
Digital tools like smartphone apps can help track macronutrients, blood glucose levels, and ketone readings. Continuous glucose monitors provide real-time data on blood sugar fluctuations. Some apps integrate with these devices for comprehensive diabetes management.
Ketone meters measure blood or breath ketones, helping individuals ensure they maintain nutritional ketosis. Regular testing is crucial for those with diabetes to prevent ketoacidosis.
Community Support and Professional Guidance
Online forums and social media groups connect individuals following a ketogenic diet for diabetes management. These communities share experiences, recipes, and tips for navigating challenges.
Local support groups offer in-person meetings to discuss diabetes management strategies. Many focus on lifestyle interventions, including dietary approaches like keto.
Working with healthcare professionals is crucial. Endocrinologists, registered dietitians, and certified diabetes educators can provide personalized guidance. They help adjust medication dosages, monitor health markers, and ensure nutritional adequacy.
Some clinics now offer specialized keto-friendly diabetes programs. These combine medical supervision with practical support for implementing and maintaining a ketogenic lifestyle.
Conclusion

The ketogenic diet shows promise as a potential approach for managing type 2 diabetes. Research indicates it can help lower blood sugar levels and promote weight loss in some individuals. The diet’s focus on reducing carbohydrate intake may lead to improved glycemic control.
Ketone bodies produced during ketosis appear to play a role in the diet’s effects. By shifting the body’s primary fuel source from glucose to fat, the keto diet can alter metabolism in ways that may benefit blood sugar regulation.
However, the long-term impacts and safety of very low-carbohydrate diets for diabetes require further study. The diet’s restrictive nature can make it challenging to follow sustainably for some people. Careful monitoring is essential, especially for those taking diabetes medications.
Nutrition therapy remains a cornerstone of diabetes management. While the ketogenic approach shows potential, it is not the only effective dietary strategy. Individualized plans considering a person’s overall health, preferences, and lifestyle are crucial.
Healthcare providers should weigh the potential benefits against risks when considering the keto diet for patients with diabetes. More research is needed to fully understand its long-term effects on health outcomes in this population.